Dr. Ashish Chhatravala
MD Pulmonary Medicine IDCCM – Critical Care
A pulmonologist or Pulmonary Disease Specialist, is a physician who possesses specialised knowledge and skill in the diagnosis and treatment of Pulmonary (Lung) conditions and diseases.
These specialists diagnose and treat conditions that affect the Pulmonary – respiratory system in men and women.
Pulmonologist have expertise in the following types of respiratory diseases :
1. Infection :
URTI
LRTI
Pneumonia
TB
2. Structural Diseases :
Bronchiectasis
Emphysema
Cystic fibrosis
3. Inflammatory Diseases :
Pulmonary fibrosis
COPD
Asthma
4. Neoplastic Diseases:
Lung cancer
5. Occupational Diseases :
Silicosis
Asbestosis
Pneumoconiosis
Occupational asthma
6. Allergic diseases:
Allergic rhinitis
Allergic asthma
7. Sleep Disorders :
OSA
OHS
In some instances this may also extends to the cardiovascular system. Certain conditions, such as pulmonary vascular disease, can affect the respiratory system but go on to affect other organ in the body.
Conditions Pulmonologist commonly treat includes:
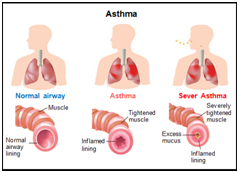
1. Asthma
A condition in which a person`s airway become inflamed, narrow and swell and produce extra mucus which makes it difficult to breath.
People may experience:
Cough – can occur at night, during exercise, can be chronic, dry, mild or severe.
Difficulty in breathing, fast breathing, frequent infection, wheezing and chest tightness.
Figure
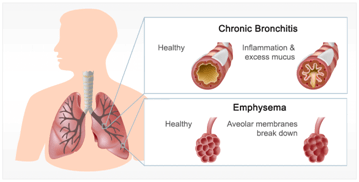
2. COPD
A group of lung diseases – an umbrella term used to describe progressive lung diseases including Emphysema, Chronic Bronchitis, Non reversible Asthma and some form of Bronchiectasis.
This disease is characterised by increasing breathlessness, coughing, sputum production, wheezing and tightness in chest.
3. Allergic rhinitis
Allergic rhinitis is a diagnosis associated with a group of symptoms affecting the nose. These symptoms occur when you breathe in something you are allergic to, such as dust, animal dander, fumes or pollen when you eat a food that you are allergic to. Symptoms include sneezing, runny nose and red, watery and itchy eyes. Sometimes over the period of time, this condition may progress to allergic asthma.
4. Tuberculosis
Tuberculosis (TB) is a potentially serious infectious disease caused by the mycobacterium tuberculosis (MTB). Tuberculosis generally affects the lungs, but can also affect other parts of the body. Most people infected with the bacteria that cause tuberculosis don’t have symptoms. When symptoms do occur, they usually include a cough (sometimes blood tinged), weight loss, night sweats and fever.
The bacteria that cause tuberculosis are spread from one person to another through tiny droplets released into the air via coughs and sneezes.
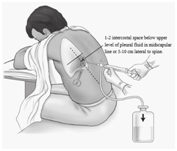
5. Pleural effusion
A pleural effusion means that there is a build up of fluid between a lung and the chest wall and separates the lung from the chest wall. A pleural effusion is a complication of various conditions. The amount of fluid varies. As the effusion become larger, it presses on the lung, which cannot expand fully when you breath. You may then become breathless. There is a large range of other symptoms that may occur, depending on the underlying cause.
6. Pneumothorax
A Pneumothorax is a collection of free air in the chest cavity (thoracic cavity) that causes the lung to collapse. Pneumothorax may occur on its own in the absence of underlying disease or as consequences of an injury or underlying lung disease. A symptomatic pneumothorax arising as a result of lung disease or injury requires immediate treatment in form of insertion of a chest tube or aspiration of free air from the chest cavity.
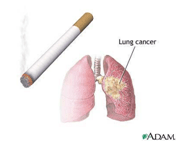
7. Lung cancer.
Lung cancer also known as lung carcinoma is a malignant lung tumour characterised by uncontrolled cell growth in tissues of the lung.
As lung cancer stages advance, symptoms includes cough, chest pain, dyspnoea, blood in sputum and weight loss.
Lung cancer is one of the most common cancers in the world and leading cause of death in men and women.
8. ILDs.
Includes a group of diseases that have thickening of the supporting tissues between the air sacs of the lungs as the commoner factor – results from a variety of causes.
ILDs usually involves all of the lungs diffusely rather than affecting only one area.
Most common symptoms of ILDs are dry cough and progressive dyspnoea.
Some forms of ILDs can lead to irreversible scarring and respiratory failure.
Prognosis depends upon the precise cause.
9. OLDs
Occupational lung diseases are occupational disease affecting the respiratory system including Occupational asthma, Coal workers Pneumoconiosis, Silicosis or Asbestosis.
Caused by inhalation of Dust, Chemical, and Vapour, Smoke, Fumes or other similar substances at work places.
The severity of the disease is related to the material inhaled and the intensity as well as duration of exposure.
Reducing exposure to harmful agents in the workplaces, in addition to reduction in cigarette smoking can help prevent a major proportion of lung diseases.
Figure
10. OSA
Sleep apnoea, is a sleep related disorders characterised by pauses in breathing or periods of shallow breathing.
When you have this condition, your breath can become very shallow or you may even stop breathing briefly while sleeping.
This type of apnoea occurs when your throat muscles intermittently relax and block your airway during sleep.
A noticeable sign of OSA is Snoring and day time sleepiness.
Treatment for OSA are available using a device that keep your airway open while you sleep.
Figure
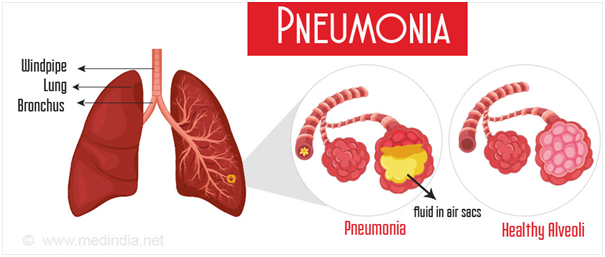
11. Pneumonia.
Infection that inflames air sacs in one or both lungs, which may fill with fluids.
Symptoms includes cough, sputum production, high grade fever with chills, chest pain and breathing difficulty in severe cases.
What Procedure Do Pulmonologist Perform?
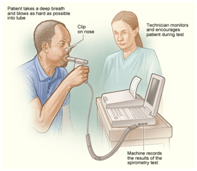
1. Spirometry – to see how well your lungs are working.
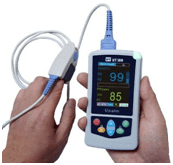
2. Pulse oxymetry test to determine the oxygen level in your blood.
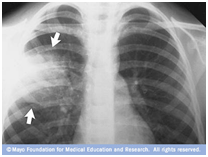
3. Chest X Ray to get gross images of the lungs, bones, muscles, fat organ and heart in your chest.
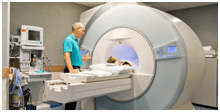
4. CT Scan to get detailed images of the lungs, bones, muscles and blood vessels in your chest.
5. Chest ultrasound to examine the organ and other chest structures.
6. Thoracocentesis to remove air or fluid from around your lungs.
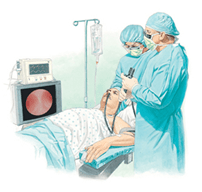
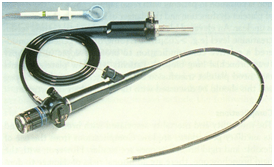
7. Bronchoscopy to examine your airway and determine if you have any issues in your throat, upper airway, larynx and lower airways. ( Diagnostic and Therapeutic).
8. Sleep study to help them diagnosed sleep related disorders such as Sleep Apnoea.
When should you see a Pulmonologist ?
If you are having any unusual symptoms like :
– Have difficulty breathing.
– Have persistent / intermittent cough.
– Regular cough up blood.
– Chest tightness.
– Occupational exposure to dust, fumes, chemicals or vapours.
– Allergic coughing, breathing problem.
– Excessive day time sleepiness and snoring with obesity.
Intensivist – critical care specialist: A Pulmonologist, Physician or Anaesthetist with special training in critical care medicine who takes care of ICU patients are referred to as Intensivist or Critical Care Specialist.
Critically ill patients include patients with life threatening single or multiple organ system failure, those at risk of clinical deterioration as well as those requiring resuscitation and / or management in Intensive care unit or High dependency Unit.
The intensive care specialist has clinical skills that include the ability to recognise and manage the disturbances associated with severe medical, surgical, obstetric and paediatric illnesses and to diagnose and treat those conditions that causes them.
This usually involves invasive and non invasive diagnostic techniques, monitoring and treatment modalities designed to support vital organs.
Intensive care specialist are also frequently involved in the management of deteriorating and seriously ill patients outside the icu, as well as during the transportation of critically ill patients.
Technologies :
Spirometry :
– Is a common office test used to assess how well your lungs work by measuring how much air you inhale, how much air you exhale.
– Use to diagnose Asthma, COPD and other respiratory conditions that affect breathing.
– May also be used periodically to check whether a treatment for chronic lung condition is helping you breath better.
– Use to conduct pre operative risk assessment before anaesthesia or cardiothoracic surgeries to predict post operative pulmonary complications.
– To diagnosed and differentiate between obstructive and restrictive lung diseases as well as for assessment of severity, prognosis and staging of the respiratory diseases.
Bronchoscopy :
Bronchoscopy is an endoscopy technique of visualisation of inside of the airway for diagnostic and therapeutic purposes.
Diagnostic :
– Abnormalities of upper and lower airways
– Obtain tissue specimen of the lung in a variety of disorders including BAL, Lung Biopsy or Endobronchial brushing.
– Therapeutic :
– To remove secretions, blood or foreign objects lodged in airway.
– Stent placement to palliate extrinsic compression of the tracheobroncheal lumen from malignant / benign processes.
– Tracheal intubation.
– Percutaneous tracheostomy.
Sleep study :
– Sleep studies are tests that record the body activity during sleep. They are helpful in identification of sleep related disorders.
– Polysomnography a type of sleep study is the gold standard to rule out OSA.
– A polysomnography study check your brain activity, eye movement, oxygen blood level, heart rate and rhythm, breathing rate and rhythm, the flow of air through your mouth and nose, the amount of snoring, body muscle movement and chest and belly movements.
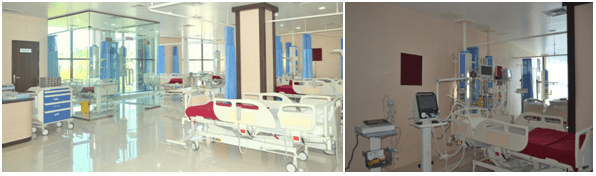
Critical Care Medicine :
– Critical care medicine or intensive care medicine, a branch of medicine concerned with the diagnosis and management of life threatening conditions that may required sophisticated organ support and invasive monitoring.
– It might treat problems such as complications from surgery, accidents, infections and severe breathing problems.
– It involves close constant attention by a team of specially trained health care specialists.
– Critical care usually takes place in an intensive care unit or trauma centre.
– So its a specialised care of patients whose conditions are life threatening and who require comprehensive care and constant monitoring.
– Using advanced therapeutic, monitoring and diagnostic technology, the objective of critical care is to maintain organ system functioning and improve the patient’s condition such that his or her underlying injury or illness can then be treated.
– ICU – Intensive care is one of the most technologically advanced and resource intensive care area of medical care. Common equipments used in an ICU includes :
– Mechanical ventilation – to assist breathing.
– Dialysis equipments for renal failure patients.
– Bedside and central hemodynamic monitoring devices.
– Defibrillator machines
– Infusion pump devices.
– Suction pumps, catheters and drains.
– Drugs including life saving medications like inotrops, sedatives, broad spectrum antibiotics and analgesics.
Under construction..